Lymphedema Surgery
Lymphedema is a condition characterized by painful swelling in the extremities (arms and/or legs). The swelling occurs when lymph nodes are no longer facilitating the proper drainage of lymph fluid from an area of the body.

Lymphedema in cancer patients
Lymphedema affects some cancer survivors who have been treated for breast cancer, gynecologic cancers, melanomas and other types of skin and urologic cancers. Lymphedema may impact cancer survivors on a daily basis and is a constant reminder of the disease that they have fought. The onset of symptoms may be delayed by months or even years after the initial injury.
Lymphedema symptoms
There are a number of symptoms that affect patients with lymphedema that typically worsen over time:
- Extremity swelling caused by lymphatic fluid
- Change in skin quality such as skin fibrosis
- Extremity tenderness or pain
- Intermittent redness of the extremity, known as cellulitis
- Excess fat in the extremity
Lymphedema treatment
Surgical treatment options for lymphedema include Lymphatic Bypass Procedures, where lymphatic vessels are connected and drained into the body’s venous system and Vascularized Lymph Node Transfer, where lymph nodes are harvested from one part of the body and surgically implanted in the affected area to rebuild a failed system.
Once the diagnosis of lymphedema is established, nonsurgical treatment is initiated as soon as possible including extremity elevation, skin care, elastic stockings, physical therapy and pneumatic compression devices. These treatments, although beneficial, can be burdensome to patients and require lifelong commitment. Surgery for lymphedema may be appropriate when nonsurgical therapy is inadequate to control the symptoms.
Questions? We got Answers!
Lymphedema is a heterogeneous disease, and treatment plans are individualized for each patient based on the clinical stage of lymphedema and anatomical considerations. During initial consultation, your surgeon may perform standardized and repeated measurements of limb circumference and refer you to specialized diagnostic testing to assist in surgical planning.
Prior to surgical therapy, the various modalities of nonsurgical treatment must be maximized including proper use of compression stockings, adherence to physical therapy recommendations, exercise and weight loss. Complete decongestive therapy (CDT) has been the mainstay of initial management for lymphedema patients.
You may be a candidate for lymphedema surgery if:
- You are able to cope well with your diagnosis and treatment
- You do not have additional medical conditions or other illnesses that may impair healing
- You have a positive outlook and realistic goals for restoring your extremity and body image
- You have maximized all nonsurgical therapies for lymphedema
Although lymphedema surgery can improve the symptoms of lymphedema, the results are highly variable:
- Visible incision lines will always be present on the extremity, depending on the type of procedure
- Certain surgical techniques will leave incision lines at the donor site, commonly located in less exposed areas of the body such as the neck, abdomen or groin region
During your lymphedema surgery consultation, be prepared to discuss:
- Your surgical goals
- Medical conditions, drug allergies and medical treatments
- Current medications, vitamins, herbal supplements, alcohol, tobacco and drug use
- Previous surgeries
Your physician will also:
- Evaluate your general health status and any pre-existing health conditions or risk factors
- Examine your extremities to assess skin quality, fibrosis and take circumferential measurements
- Take photographs
- Discuss your options and recommend a course of treatment
- Discuss likely outcomes of lymphedema surgery and any risks or potential complications
Be sure to ask your physician questions. It’s very important to understand all aspects of your type of lymphedema and potential treatments.
In preparing for lymphedema surgery, you may be asked to:
- Get lab testing or a medical evaluation
- Take certain medications or adjust your current medications
- Obtain specialized diagnostic testing and imaging such as ICG
- lymphography
- Stop smoking
- Achieve weight loss goals
- Avoid taking aspirin, anti-inflammatory drugs and herbal supplements as they can increase bleeding
Lymphedema surgery is typically performed in a hospital setting, may include a short hospital stay, and will likely use general anesthesia. Some follow-up procedures may be performed on an outpatient basis, and local anesthesia with sedation may be used.
These decisions will be based on the requirements of your specific procedure and in consideration of your preferences and your doctor’s best judgment.
Lymphaticovenular anastomosis
Lymphaticovenular anastomosis (LVA) is a bypass procedure that redirects excess lymphatic fluid into the venous circulation within the arm or leg. Small, superficial incisions are made on the extremity, and a powerful surgical microscope is used to identify tiny lymphatic vessels beneath the skin. Once located, these lymphatic vessels can be connected to nearby small blood vessels (venules). As many lymphaticovenular connections as possible are created to facilitate shunting of fluid. This procedure is often performed on an outpatient basis.
Vascularized lymph node transfer
In situations when lymph node basins do not function, such as after lymph node dissection or radiation therapy, vascularized lymph node transfer (VLNT) can promote lymphatic drainage. Donor lymph nodes can be harvested from a variety of locations such as the lower abdomen and neck. This procedure typically uses microsurgery techniques to transfer lymph nodes and fatty tissue with their blood supply. This procedure typically requires hospitalization for a few days.
Women who are seeking simultaneous breast reconstruction and treatment of arm lymphedema due to breast cancer may be candidates for autologous breast reconstruction using lower abdominal flaps (such as DIEP flap) with attached lymph nodes.
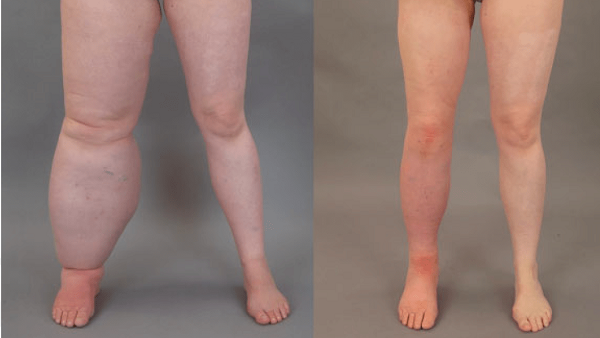
Ablative procedures
Ablative procedures aim to remove excess skin and soft tissue to decrease bulk and facilitate hygiene. These operations are usually reserved for patients with advanced-stage lymphedema with significant fibrosis and fatty infiltration. Removal of redundant skin with this technique may require more than one surgery. More recently, liposuction has been successfully used to treat patients with advanced lymphedema with excess fat who are not candidates for lymphaticovenular anastomosis or lymph node transfer. It is important to recognize that patients must be committed to lifelong compression garments to maintain the effects of liposuction.
Following lymphedema surgery, gauze or bandages may be applied to your incisions. A small, thin tube may be temporarily placed under the skin to drain any excess blood or fluid following flap procedures.
You will be given specific instructions that may include: How to care for your surgical site(s) following surgery, medications to apply or take orally to aid healing and reduce the risk of infection, specific concerns to look for at the surgical site or in your general health and when to follow up with your plastic surgeon.
Be sure to ask your plastic surgeon specific questions about what you can expect during your individual recovery period.
- Where will I be taken after my surgery is complete?
- What medication will I be given or prescribed after surgery?
- Will I have dressings/bandages after surgery? When will they be removed?
- Will there be drains? For how long?
- When can I bathe or shower?
- When can I resume normal activity and exercise?
- When can I resume nonsurgical therapies for lymphedema?
- When do I return for follow-up care?
Healing will continue for several weeks while swelling decreases. Continue to follow your plastic surgeon’s instructions and attend follow-up visits as scheduled.
The long-term results of lymphedema surgery can help lessen the physical and emotional impact of lymphedema. Many patients experience reduction in extremity circumference or volume over several months after surgery. In addition, other symptoms such as extremity tightness and heaviness may improve after surgery. Aggressive nonsurgical therapies are advised after surgery to maintain the best outcomes, depending on the type of procedure performed. If the lymphedema improves, patients may gradually decrease their dependence on nonsurgical strategies. If lymphedema worsens, additional surgical interventions can be considered.